Arteriovenous Malformations
AVM Basics
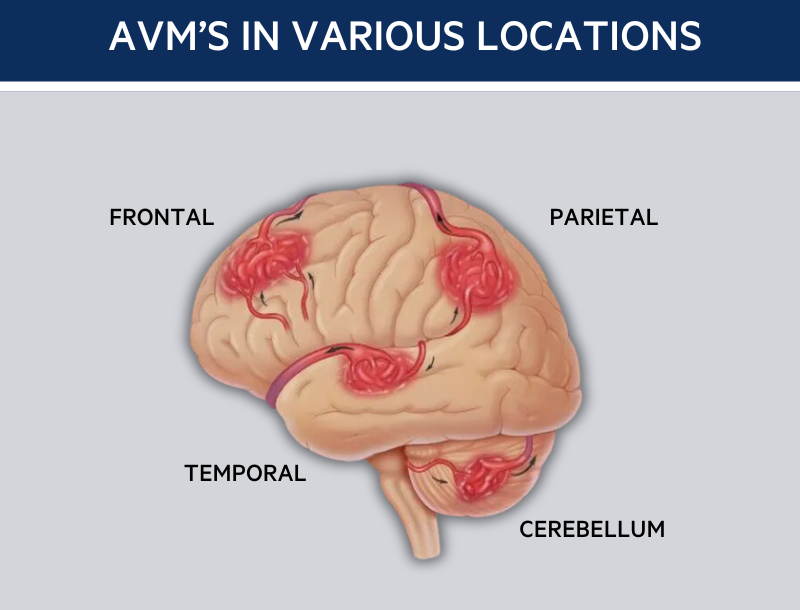
An arteriovenous malformation (AVM) is a tangle of abnormal blood vessels connecting arteries and veins via fistulas or shunts. Brain AVMs are the most common, affecting about 18 in 100,000 people in the U.S., although only 1 in 100,000 are diagnosed.
In brain AVMs, high-pressure arterial blood flows directly into veins, bypassing the capillary bed that nourishes brain tissue and reduces blood pressure. This can cause vessel expansion, potentially leading to an aneurysm, which may rupture and cause a hemorrhagic stroke.
AVMs are found during routine exams in 5-10% of cases, but about half are discovered after a hemorrhage. Symptoms include sudden/severe headaches, nausea/vomiting; seizure; and symptoms normally associated with having a stroke, such as difficulties with speech, movement, or vision
Bleeding from an AVM causes temporary or permanent brain damage in 20-30% of cases, leading to paralysis, weakness, or difficulties with speech, memory, or sight, and results in death in 10-15% of cases. AVMs affect males and females equally, usually diagnosed between ages 20-60, though they can also be present at birth and diagnosed in children. Additionally, 10-60% of patients with AVMs have brain aneurysms.
Cause of AVMs
The cause of AVMs is not yet understood. Most experts believe that AVMs develop during fetal development and therefore exist at birth (known as a congenital condition), however it is possible that some AVMs develop after birth.
AVMs are not an inherited condition (with the exception of an inherited condition called Hereditary Hemorrhagic Telangiectasia, or HHT, which increases the risk of developing AVMs 10,000-fold).
Diagnosis
If an AVM is suspected, a variety of tests are available to make the diagnosis and establish its location and size and also whether it has hemorrhaged, which helps doctors determine the optimal treatment. These tests include, CT scans, MRI scans, and angiograms.
Treatment
The goal of AVM treatment is to prevent hemorrhage, with an annual risk of 2-4%, higher if previously occurred. The risk exists even without symptoms. Treatment decisions consider the patient’s age, health, AVM location and size, and symptoms.
Major Treatments:
- Surgery (microsurgical resection): Invasive procedure to remove the AVM, performed under general anesthesia. Hospital stay is typically four to six days, with at least one day in the ICU.
- Stereotactic Radiosurgery: Non-invasive, uses focused radiation beams to destroy the AVM over about three years. Effective for small AVMs or those in critical brain areas. Completed in one to three sessions with a 70-80% success rate.
- Embolization (endovascular surgery): Minimally invasive, uses materials to plug blood vessels supplying the AVM via a catheter. Often combined with surgery or radiosurgery to reduce AVM size.
- Medical Management: Regular monitoring and symptom management, suitable for patients with high surgical risks or large AVMs in critical brain areas.
* Illustration © 2007 Chris Gralapp
* Licensed exclusively to The Aneurysm and Foundation (TAAF )


 Brain Aneurysm Foundation
Brain Aneurysm Foundation